We all do it. It’s a natural part of life, yet most people don’t feel comfortable discussing it openly. Yes, we’re talking about your stool, and it has much more to say about your health than you might realize.
Your bowel movements can provide valuable insights into your digestive system and overall health. From color and consistency to frequency and smell, your stool can signal everything from minor digestive issues to more serious health concerns that might require medical attention.
In this guide, we’ll break down what your stool can tell you about your health, when variations from normal are cause for concern, and when it’s time to consult a gastroenterologist.
Why Your Stool Is an Important Health Indicator
Think of your stool as a window into your digestive system. It can reveal how well your body is processing food, absorbing nutrients, and eliminating waste. Changes in your stool can reflect digestive efficiency, hydration levels, gut microbiome health, potential inflammation, possible infections, diet changes, and medication effects.
The journey of food through your digestive system begins in your mouth, where enzymes start breaking down carbohydrates. As food travels through your stomach and small intestine, proteins and fats are broken down, and nutrients are absorbed. By the time waste reaches your large intestine, most nutrients have been extracted, leaving behind indigestible fibers, water, and bacteria. Your colon absorbs excess water, and the resulting waste becomes stool.
This entire process typically takes between 24 and 72 hours, and the characteristics of your stool, its color, consistency, size, shape, and smell can provide valuable clues about how efficiently this process is working. It can also offer insights into potential issues along the digestive tract, from your oesophagus to your rectum.
Paying attention to what’s normal for you makes it easier to spot when something changes and whether that change might signal a health issue worth investigating.
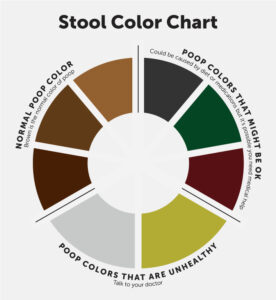
Decoding Stool Color: What Each Shade Means
The color of your stool can vary based on what you eat, medications you take, and how quickly food moves through your digestive system. Here’s what different colors might indicate:
Brown (Various Shades)
What it means: This is the normal, healthy color resulting from bile and bilirubin, which are released during digestion. Bile starts green in the gallbladder but turns brown as it passes through the digestive tract and interacts with enzymes and bacteria in your intestines. The specific shade of brown can vary depending on your diet and how long the stool remains in your colon.
When to be concerned: Generally not a concern unless accompanied by other symptoms. However, persistent changes in shade that can’t be attributed to diet might warrant attention, especially if coupled with other digestive issues like abdominal pain, bloating, or changes in bowel habits.
Green
What it means: Often caused by eating green vegetables, food coloring, or iron supplements. Chlorophyll in leafy greens like spinach and kale can give stool a greenish tint. It can also occur when food moves through your digestive tract too quickly, not giving bile enough time to break down completely. This rapid transit might happen during episodes of diarrhea or after consuming certain foods that accelerate digestion.
When to be concerned: Usually not concerning unless persistent without explanation. If you haven’t consumed green foods or supplements and experience ongoing green stools, it might be worth discussing with a healthcare provider, especially if accompanied by diarrhea or stomach discomfort.
Black
What it means: Can be caused by certain foods (licorice, blueberries, blackberries), supplements (iron, activated charcoal), or medications (Pepto-Bismol, which contains bismuth subsalicylate that can turn stool black). The darkening occurs due to chemical reactions between these substances and digestive enzymes or direct pigmentation from the ingested materials.
When to be concerned: When it’s tarry and sticky (melena), which could indicate bleeding in the upper digestive tract, such as from an ulcer, gastritis, or varices. This requires immediate medical attention. The black, tarry appearance results from blood being exposed to digestive enzymes as it travels through your intestines, causing the hemoglobin to break down and darken.
Red or Maroon
What it means: Could be from red foods (beets, tomato juice, red gelatin), food coloring, or certain medications. The vibrant pigments in these foods can pass through your digestive system relatively unchanged, temporarily coloring your stool.
When to be concerned: When not attributable to diet, as it could indicate bleeding in the lower digestive tract (large intestine, rectum) or hemorrhoids. Fresh blood appears red because it hasn’t been exposed to digestive enzymes long enough to break down and change color. Seek prompt medical advice, as this could indicate conditions like inflammatory bowel disease, diverticulosis, polyps, or even colorectal cancer.
Yellow
What it means: May indicate excess fat in the stool, which could point to malabsorption issues. When your body can’t properly absorb fats, they pass through your digestive system and give stool a yellowish, greasy appearance. This can happen due to deficiencies in digestive enzymes or conditions affecting the pancreas, gallbladder, or liver.
When to be concerned: When consistently yellow, greasy, and foul-smelling, especially if accompanied by weight loss, abdominal pain, or bloating. These symptoms might suggest conditions like celiac disease, pancreatic insufficiency, or gallbladder problems that prevent proper fat digestion and absorption.
Pale or Clay-Colored
What it means: May suggest a bile duct obstruction or liver issues. Bile gives stool its characteristic brown color, so when bile production or flow is inhibited, stool can appear pale, clay-colored, or grayish. This can happen due to gallstones blocking bile ducts, liver disease affecting bile production, or certain medications interfering with normal liver function.
When to be concerned: Consistently pale stools warrant a doctor’s visit, as they could indicate problems with your liver, gallbladder, or pancreas. When accompanied by yellowing of the skin or eyes (jaundice), dark urine, or abdominal pain, it might suggest serious liver or biliary conditions requiring prompt medical evaluation.
The Bristol stool chart: Types of poop and what they mean
Let’s face it: talking about your bathroom habits isn’t exactly everyone’s favorite conversation topic, especially when you’re sitting in a doctor’s office. But it’s an important part of monitoring your health. The Bristol Stool Chart simplifies these conversations by categorizing bowel movements into seven distinct types based on shape and consistency. Developed by medical researchers, this chart helps both patients and doctors communicate clearly about digestive health without awkward descriptions. While everyone experiences different stool types occasionally, consistently seeing types that indicate constipation or diarrhea might signal it’s time to consult a healthcare professional. This guide will help you understand what your body is telling you and when you should seek medical advice.
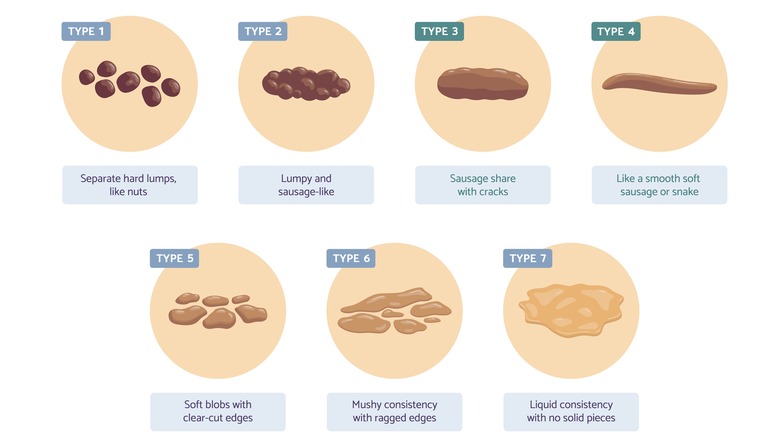
Types of Stool on the Bristol Stool Chart:
Type 1
Separate hard lumps, like nuts (hard to pass)
What it means: These stools indicate severe constipation. It means you’re dehydrated or not eating enough fiber. Your stool remains in your colon for too long, and excess water is absorbed, causing it to become hard and difficult to pass.
What to do: Increase water intake and fiber-rich foods like fruits, vegetables, and whole grains. Regular physical activity can also help keep things moving.
Type 2
Lumpy and sausage-like
What it means: This is also a sign of mild to moderate constipation. Your stool is formed, but it’s still quite firm.
What to do: Try to increase your fiber intake and drink plenty of fluids to soften the stool. Exercise and avoiding stress can also help with regular bowel movements.
Type
Like a sausage but with cracks on the surface.
What it means: This stool type is normal and indicates healthy digestion. It’s well-formed, not too hard, not too soft.
What to do: Keep up with a balanced diet and hydration to maintain healthy digestion.
Type 4
Like a smooth, soft sausage or snake
What it means: This is the ideal stool—the most typical and healthiest form. It suggests that you have a balanced diet with adequate fiber and hydration.
What to do: Continue maintaining a fiber-rich diet and drink plenty of water to keep everything running smoothly.
Type 5
Soft blobs with clear-cut edges (passed easily)
What it means: This type could indicate mild diarrhea or that your body is not absorbing nutrients as well as it should.
What to do: Keep track of your symptoms, and consider adjusting your diet (avoiding excess fatty foods or caffeine) or seeking advice from a healthcare provider.
Type 6
Fluffy pieces with ragged edges, a mushy stool
What it means: This is a sign of mild diarrhea, possibly caused by a diet high in fat or sugar, stress, or a mild gastrointestinal infection.
What to do: Stay hydrated, and if diarrhea persists, avoid triggers like greasy or spicy foods. If it continues for more than a few days, consult a doctor.
Type 7
Watery, no solid pieces (entirely liquid)
What it means: This indicates severe diarrhea. It may be caused by infection, food intolerances, stress, or certain medications.
What to do: Replenish fluids and electrolytes to prevent dehydration. If this continues, especially if accompanied by other symptoms like fever or vomiting, seek medical attention.
Your stool’s position on this chart can reveal valuable information about your digestive function, hydration status, and even potential health issues. Consistently hard stools might suggest dehydration or insufficient fiber, while chronic loose or watery stools could indicate inflammation, infection, or food intolerances.
By becoming familiar with the Bristol Stool Chart and identifying your typical patterns, you can better recognize when changes occur and determine whether they might be related to dietary choices, hydration levels, medication effects, or potential health concerns.
Frequency and Smell: What’s Normal?
Frequency
There’s no single “normal” frequency for bowel movements. The range can vary from three times a day to three times a week, depending on the individual. Factors influencing this include diet, physical activity, age, hormonal fluctuations, and even stress levels.
Some people are as regular as clockwork, having bowel movements at roughly the same time each day. Others experience more variability. Both patterns can be entirely normal, provided they’re consistent for the individual and don’t cause discomfort or other symptoms.
What’s most important is that your personal pattern’s significant changes from your usual routine might indicate a problem. For example, if you typically have a bowel movement daily but suddenly go several days without one, or if you start having multiple loose stools when that’s not your norm, it’s worth paying attention to these changes, especially if they persist.
Smell
Let’s be honest, stool never smells pleasant. The characteristic odor comes from the normal bacterial fermentation process in your gut and the breakdown of various compounds during digestion. However, a dramatic change in odor could indicate infections, malabsorption issues, certain medical conditions, or diet changes.
Foods high in sulfur, such as garlic, onions, and certain vegetables, can make your stool particularly pungent. Similarly, animal proteins can produce stronger-smelling bowel movements. These dietary influences are typically temporary and not cause for concern.
However, unusually foul-smelling stools that persist, particularly when described as putrid or rotten, might suggest digestive issues like malabsorption syndromes, where nutrients aren’t properly absorbed and instead ferment in the gut. Conditions like celiac disease, inflammatory bowel disease, or infections can cause this change in odor.
Your typical diet, gut flora, and digestive efficiency all influence the scent of your stool. While unpleasant odors are normal, unusually foul smells that persist may warrant attention, especially when accompanied by other changes like altered consistency, color, or frequency.
Red Flags: When to Be Concerned
While minor, temporary changes in your stool are usually not cause for alarm, certain symptoms warrant attention. Blood in the stool, whether bright red, maroon, or black, should never be ignored as it could indicate anything from hemorrhoids to more serious conditions like inflammatory bowel disease, diverticulitis, polyps, or colorectal cancer. The location of bleeding often influences the color. Upper digestive tract bleeding typically appears black or tarry, while lower tract bleeding tends to be bright red or maroon.
Persistent diarrhea lasting more than two days can lead to dehydration and may signal an infection, an inflammatory condition, or food intolerance. Continuous loose stools deplete your body of important fluids and electrolytes, potentially leading to weakness, dizziness, and other complications, especially in vulnerable populations like children and the elderly.
Severe or chronic constipation can cause discomfort and might be linked to dietary issues, medication side effects, or underlying health conditions such as hypothyroidism, diabetes, or neurological disorders. When constipation becomes chronic, it can lead to complications like hemorrhoids, anal fissures, or even fecal impaction in severe cases.
Unexplained weight loss accompanying stool changes could point to malabsorption or more serious digestive disorders like inflammatory bowel disease, celiac disease, or malignancies affecting the digestive tract. When your body cannot properly absorb nutrients from food, weight loss often follows, even without intentional dietary changes.
Severe pain during bowel movements is never normal and requires medical evaluation. It might indicate conditions like anal fissures, abscesses, severe hemorrhoids, or inflammatory processes affecting the rectum or anus. The pain should not be dismissed as merely a consequence of constipation or diarrhea if it’s severe or persistent.
Narrow, pencil-thin stools, especially if this is a new change, might indicate an obstruction or narrowing in the colon due to inflammation, scarring, or masses. When stool has to pass through a narrowed section of the intestine, it takes on this characteristic thin shape, potentially signaling conditions requiring prompt investigation.
Pale or clay colored stools often suggest bile duct issues, which can stem from gallstones, tumors, or inflammation affecting the biliary system. Since bile gives stool its characteristic brown color, problems with bile production or flow can result in these lighter-colored bowel movements.
Dark urine accompanying light-colored stools further supports potential liver or bile duct problems and requires prompt medical attention. This combination often suggests that bilirubin, which normally exits the body via bile and stool, is instead being processed through the kidneys and urine due to biliary obstruction.
Stay on Top of Colorectal Cancer Screenings
Regular colorectal cancer screenings are essential for early detection and prevention. The American Cancer Society recommends that people at average risk of colorectal cancer begin regular screenings at age 45.
Colorectal cancer often begins as small, noncancerous (benign) clumps of cells called polyps that form on the inside of the colon. Over time, some of these polyps can develop into cancer. Screenings can help doctors find and remove polyps before they turn cancerous.
When to Consult a Gastroenterologist
You should schedule an appointment with a gastroenterologist if you experience any red flag symptoms mentioned above. Gastroenterologists are specialized physicians who focus exclusively on the digestive system and its disorders, making them uniquely qualified to evaluate and treat issues affecting your gastrointestinal tract.
Persistent changes in bowel habits lasting more than two weeks deserve professional evaluation, even if they seem minor. Our bodies typically establish relatively consistent patterns, so prolonged departures from your normal routine could signal underlying issues requiring attention.
Those with a family history of colorectal cancer or inflammatory bowel disease who develop new digestive symptoms should seek care promptly. Genetic factors play a significant role in these conditions, and early detection can dramatically improve outcomes, particularly for colorectal cancer, which responds well to early treatment.
Ongoing abdominal pain or discomfort that doesn’t resolve with basic interventions warrants investigation. While occasional digestive discomfort is common, persistent pain might indicate conditions like irritable bowel syndrome, inflammatory bowel disease, or other disorders requiring specific diagnosis and management.
Unexplained fatigue alongside digestive symptoms could indicate nutritional deficiencies or chronic conditions affecting nutrient absorption. Conditions like celiac disease, Crohn’s disease, or ulcerative colitis can impact your body’s ability to extract essential nutrients from food, leading to fatigue, weakness, and other systemic symptoms.
Heartburn or acid reflux that doesn’t respond to over-the-counter treatments might suggest more complex issues requiring specialized care. Gastroesophageal reflux disease (GERD), Barrett’s esophagus, or hiatal hernias might need prescription medications or other interventions that a gastroenterologist can provide.
Don’t delay seeking help due to embarrassment. Gastroenterologists are medical professionals who specialize in digestive health and have seen it all before. Their expertise can provide relief and prevent complications from undiagnosed digestive conditions. Most people find that once they overcome initial hesitation, discussing digestive symptoms becomes much easier, especially with specialists who approach these topics professionally and routinely.
Keeping Your Digestive System Healthy
While being observant about your stool is important, maintaining good digestive health involves several lifestyle factors. Staying hydrated by drinking plenty of water supports proper digestion and soft, regular bowel movements. Most health authorities recommend consuming at least eight 8-ounce glasses of water daily, though individual needs may vary based on activity level, climate, and overall health.
Eating a fiber-rich diet with plenty of fruits, vegetables, and whole grains provides the bulk needed for healthy stool formation and regular elimination. Dietary fiber helps maintain bowel regularity by adding bulk and softness to stool, making it easier to pass. Aim for 25-30 grams of fiber daily, gradually increasing your intake to avoid bloating or gas that can accompany sudden dietary changes.
Regular exercise stimulates intestinal contractions and helps maintain optimal digestive function. Physical activity encourages more efficient movement of food through your digestive tract, reducing transit time and potentially preventing constipation. Even moderate exercise like walking for 30 minutes daily can significantly benefit digestive health.
Managing stress through mindfulness, meditation, or other techniques can reduce digestive disturbances, as the gut-brain connection is powerful and well-established. The digestive system has its nervous system, often called the “second brain,” which communicates closely with your central nervous system. Stress and anxiety can trigger or worsen symptoms like abdominal pain, bloating, diarrhea, or constipation through this connection.
Limiting alcohol consumption protects the digestive tract from irritation and inflammation. Alcohol can damage the delicate lining of your stomach and intestines, potentially leading to issues like gastritis, ulcers, or malabsorption. It can also disrupt the balance of beneficial bacteria in your gut, affecting overall digestive health.
Avoiding smoking prevents numerous digestive complications, from acid reflux to increased cancer risk. Smoking weakens the lower esophageal sphincter, allowing stomach acid to flow backward into the esophagus. It also increases the risk of various digestive cancers, including those affecting the esophagus, stomach, pancreas, and colon.
Taking probiotics, if recommended by your healthcare provider, may support a healthy gut microbiome and improve overall digestive wellness. These beneficial bacteria help maintain a balanced intestinal environment, potentially improving digestion, enhancing immune function, and even influencing mood through the gut-brain axis.
The Bottom Line
Paying attention to your stool might not be the most glamorous aspect of health monitoring, but it provides valuable insights into your digestive system and overall well-being. By understanding what’s normal for you, recognizing warning signs, and knowing when to seek medical advice, you can take a proactive approach to your health.
Your digestive system processes approximately 30 tons of food over an average lifetime, extracting nutrients that fuel every cell in your body while eliminating waste efficiently. This remarkable system deserves attention and care, particularly since digestive disorders affect an estimated 60-70 million Americans annually, according to the National Institutes of Health.
Remember: when it comes to digestive health, there’s no such thing as a silly question or concern. If you notice persistent changes in your stool or experience any red flag symptoms, don’t hesitate to reach out to a gastroenterologist. Early detection and treatment of digestive issues can make a significant difference in your long-term health outcomes, potentially preventing complications and improving quality of life.
Regular screenings are also essential, particularly for colorectal cancer, which remains one of the most preventable yet still common cancers in the United States. Following recommended screening guidelines—typically beginning at age 45 for average-risk individuals—can lead to early detection of polyps before they develop into cancer or identify cancer at its most treatable stages.
This article is for informational purposes only and should not replace professional medical advice. Always consult with a healthcare provider regarding any health concerns.
Have you noticed changes in your stool that concern you? Schedule a consultation with a gastroenterologist today to discuss your digestive health.
