Imagine having persistent stomach pain and bleeding that doctors can’t explain despite multiple tests. Traditional endoscopy procedures require sedation, uncomfortable tubes, and time off work, yet they still can’t examine your entire small intestine. Capsule endoscopy changes this equation entirely, offering a complete view of your digestive tract by simply swallowing a pill-sized camera.
This revolutionary diagnostic tool has transformed gastroenterology, providing answers for thousands of patients who previously faced uncertain diagnoses and repeated invasive procedures.
What Is Capsule Endoscopy?
Capsule endoscopy uses a vitamin-sized device containing a miniature camera, LED lights, a battery, and a wireless transmitter. Measuring just 11mm wide by 26mm long, this sophisticated capsule travels naturally through your digestive system, capturing 2-6 high-resolution images per second for 8-12 hours.
The technology addresses a critical gap in traditional diagnostics. Upper endoscopy only reaches the first portion of your small intestine, while colonoscopy examines the large intestine and the very end of the small intestine. This leaves more than 25 feet of small intestine, where many conditions hide largely unexamined until now.
Modern capsules come in different varieties. Small bowel capsules are most common, providing comprehensive small intestine imaging. Colon capsules offer an alternative to traditional colonoscopy for specific patients, though they require more extensive preparation. Some newer capsules even include pH sensors and medication delivery capabilities.
Advanced Technology Behind the Camera
Once swallowed, the capsule moves through your system via natural muscle contractions called peristalsis. Its multiple LED lights illuminate the dark intestinal environment while the high-definition camera captures detailed images using CMOS technology similar to smartphone cameras, but miniaturized to fit the capsule’s constraints.
These images transmit wirelessly to a data recorder worn on your belt, storing thousands of pictures throughout the day. The recorder uses advanced algorithms to ensure no images are lost during transmission, even if you move around normally during the procedure.
After the capsule passes naturally from your body within 1-3 days, doctors download the images and review them as a continuous video. Specialized software helps identify abnormalities, inflammation, bleeding sources, and other diagnostic clues. Some systems now incorporate artificial intelligence to assist physicians in detecting subtle abnormalities that might be missed during manual review.
The image quality has improved dramatically since the first capsules were introduced in 2001. Modern devices can detect lesions as small as a few millimeters and provide detailed views of the intestinal surface texture, blood vessels, and any inflammatory changes.
Medical Conditions It Diagnoses
Capsule endoscopy excels at detecting small bowel conditions that traditional methods often miss. It’s particularly valuable for unexplained gastrointestinal bleeding, where the source frequently lies hidden in the small intestine. Studies show capsule endoscopy identifies bleeding sources in 60-70% of cases where traditional endoscopy found nothing.
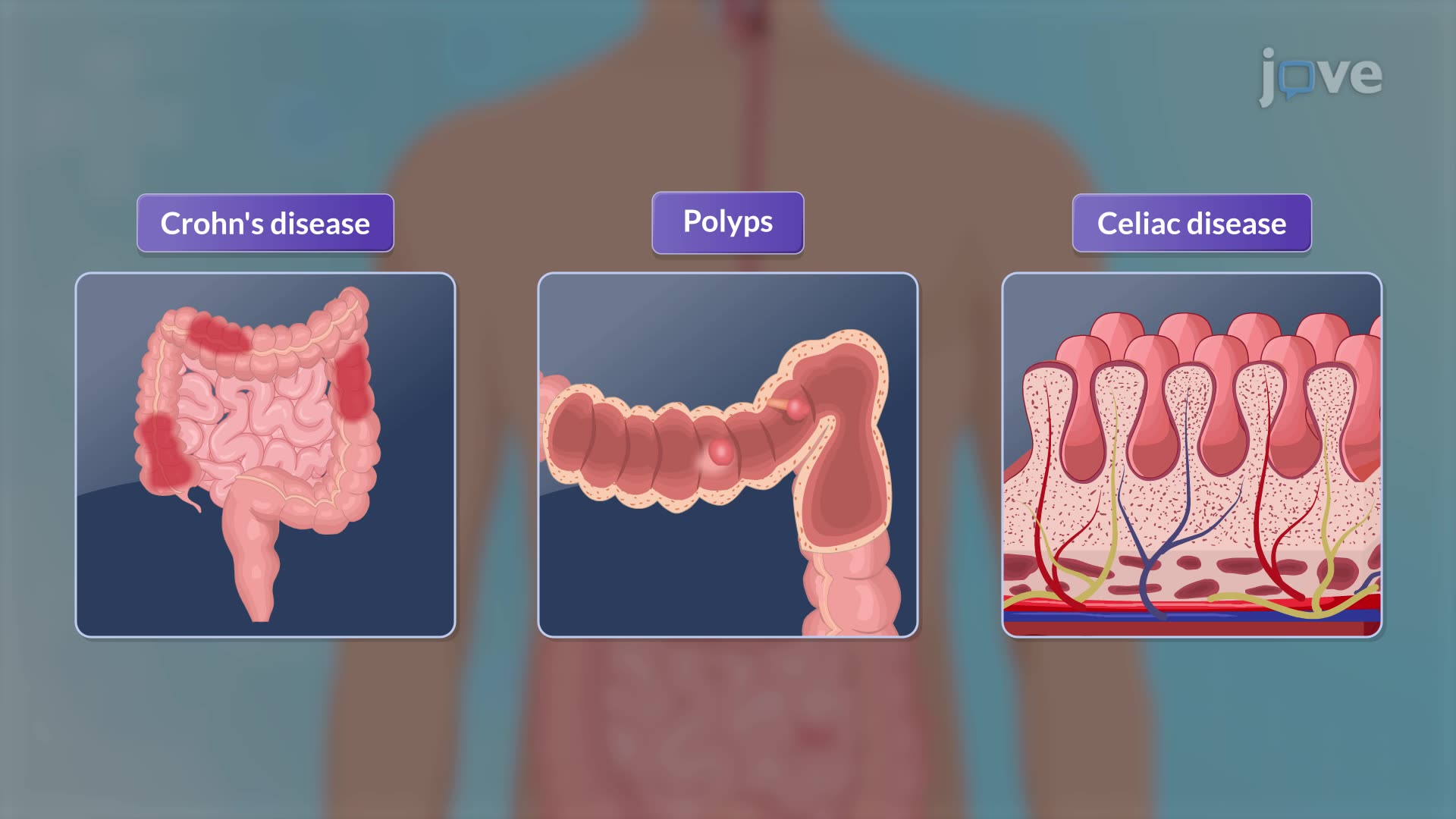
For Crohn’s disease, capsule endoscopy reveals early inflammation, assesses disease extent, and monitors treatment response. It can detect subtle mucosal changes that precede visible inflammation on other imaging studies. The procedure often provides definitive diagnosis when other tests show normal results, potentially changing treatment approaches and improving patient outcomes.
Similarly, it evaluates celiac disease damage extent and tracks healing progress after gluten-free diet adoption. This is particularly valuable for patients with refractory celiac disease who aren’t responding to dietary changes as expected.
The technology also detects small bowel tumors, both benign and malignant, that conventional endoscopy cannot reach. While small bowel cancers are relatively rare, representing only 3% of gastrointestinal malignancies, early detection significantly impacts treatment success. Capsule endoscopy can identify benign polyps, pre-malignant adenomas and early cancers that might otherwise go undetected for months or years.
For patients with iron deficiency anemia from unknown sources, capsule endoscopy frequently identifies small bleeding lesions causing chronic blood loss. This is particularly important in elderly patients, where small vascular malformations called angioectasias are common causes of slow, chronic bleeding.
Other conditions effectively diagnosed include small bowel strictures, medication-induced enteropathy, hereditary polyposis syndromes, and monitoring of known small bowel conditions. Research continues to expand applications, including the evaluation of functional disorders and medication absorption patterns.
A health care professional might suggest a capsule endoscopy procedure to:
- Find the cause of bleeding in the small intestine. This is the most common reason for doing a capsule endoscopy.
- Diagnose inflammatory bowel diseases. Capsule endoscopy can find the irritated and inflamed areas in the small intestine in diseases such as Crohn’s disease or ulcerative colitis.
- Diagnose cancer. Capsule endoscopy can show tumors in the small intestine or other parts of the digestive tract.
- Diagnose celiac disease. Capsule endoscopy is sometimes used in diagnosing and monitoring this immune reaction to eating gluten.
- Look at the esophagus. Capsule endoscopy can review the muscular tube that connects the mouth and the stomach, called the esophagus. This is to look for veins that have gotten larger, called varices.
- Screen for polyps. Certain syndromes that run in families can cause polyps in the small intestine. A capsule endoscopy can check for these polyps.
- Do follow-up testing after X-rays or other imaging tests. If the results of an imaging test are unclear, a capsule endoscopy might provide more information.
The Complete Patient Experience
Preparation is minimal compared to traditional procedures. Most patients follow a clear liquid diet for 12-24 hours beforehand, with no bowel-cleansing solutions typically required. Some physicians may prescribe a mild laxative to optimize visualization, but the preparation is far gentler than colonoscopy requirements.
Your doctor will review your medication list before the procedure. Some medications, particularly those affecting intestinal motility, may need temporary adjustment. Iron supplements are typically stopped several days before the procedure as they can interfere with image quality.
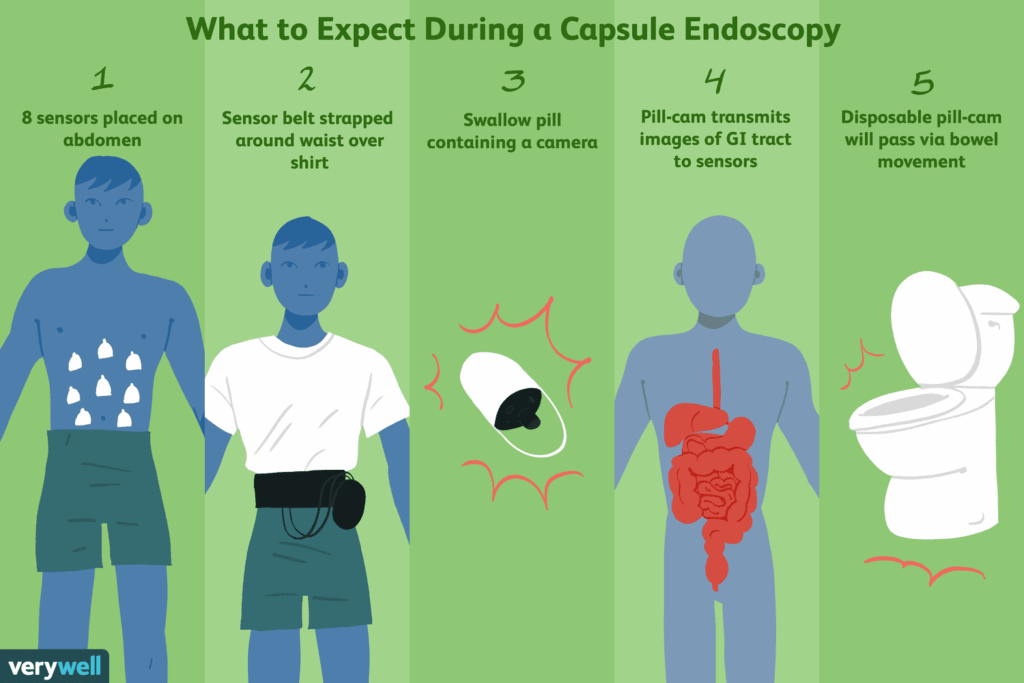
On procedure day, you’ll arrive at the medical facility where technicians attach sensor patches to your abdomen and fit you with the lightweight data recorder belt. The recorder, roughly smartphone-sized, is surprisingly unobtrusive and can be worn under clothing. The sensor patches contain antennae that receive wireless signals from the capsule as it travels through your system.
Swallowing the smooth capsule feels like taking a large vitamin. The capsule’s surface is specially designed to be slippery when wet, making it easy to swallow with water. After a two-hour waiting period to allow the capsule to exit your stomach, you can eat a light snack and resume normal activities.
The eight-hour recording period allows you to work, run errands, or relax at home. The only restrictions involve avoiding strenuous exercise that might interfere with signal transmission, staying within a reasonable distance of the medical facility, and avoiding MRI machines during the recording period. Most patients report that they quickly forget about the procedure and go about their normal day.
Some patients experience mild sensations as the capsule moves through their system, but most feel nothing at all. The capsule’s journey is entirely passive, moved along by your body’s natural digestive processes.
At day’s end, you return to have the recorder and sensor patches removed. The capsule continues its journey and is eliminated naturally with a bowel movement, usually within 24-72 hours. Unlike some medical devices, the capsule doesn’t need to be retrieved – it’s designed for normal disposal.
Results are typically available within 3-7 days, depending on the complexity of findings and your physician’s schedule. Your gastroenterologist will provide a comprehensive report of their findings, often including still images of any abnormalities discovered.
Significant Advantages Over Traditional Methods
Capsule endoscopy eliminates sedation risks entirely. Traditional endoscopic procedures typically require conscious sedation or general anesthesia, carrying inherent cardiovascular and respiratory risks, particularly for elderly patients or those with underlying health conditions. This sedation-free approach makes the procedure accessible to patients who might not be candidates for traditional endoscopy.
The comfort factor cannot be overstated. Unlike traditional endoscopy’s flexible instruments that can cause gagging, throat irritation, or abdominal cramping, swallowing a capsule involves no physical discomfort during or after the procedure. There’s no sore throat, no recovery period, and no restrictions on driving or working afterward.
Complete small intestine visualization sets capsule endoscopy apart from all other diagnostic methods. While traditional methods leave more than 25 feet of small intestine unseen, capsule endoscopy provides comprehensive coverage that ensures hidden lesions, inflammation, or bleeding sources are likely detected rather than missed. Studies consistently show that capsule endoscopy identifies small bowel abnormalities in 60-80% of patients with negative conventional endoscopy results.
The procedure carries virtually no perforation risk since no instruments navigate your digestive tract. Traditional endoscopy, while generally safe, carries a small but real risk of perforation, bleeding, or other complications related to instrument manipulation.
From a practical standpoint, the convenience is remarkable. There’s no need to take time off work beyond the initial setup and final recorder removal. No transportation arrangements are necessary since there’s no sedation. Many patients schedule the procedure around their workday with minimal disruption.
Psychologically, many patients find capsule endoscopy far less anxiety-provoking than traditional procedures. This reduced anxiety makes patients more likely to undergo necessary testing and maintain regular healthcare, potentially leading to earlier diagnosis and better outcomes.
Important Limitations and Considerations
Capsule endoscopy is purely diagnostic. If abnormalities are discovered, additional procedures may be needed for tissue sampling, polyp removal, or therapeutic interventions. This means some patients may ultimately require traditional endoscopy anyway, though the capsule results help guide these procedures more precisely.
Image quality can occasionally be compromised by factors beyond anyone’s control. Rapid intestinal transit, poor preparation, or intestinal contents can result in suboptimal visualization of certain areas. Unlike traditional endoscopy, where physicians can irrigate, suction, or adjust positioning for better views, capsule endoscopy relies entirely on natural conditions within your digestive tract.
Capsule retention occurs in less than 2% of procedures overall but represents the most serious potential complication. This happens when the capsule lodges in narrowed intestinal areas, usually from Crohn’s disease strictures, tumors, or previous surgical scarring. Retention rates are higher in patients with known small bowel strictures, sometimes reaching 5-10% in high-risk populations.
Most retained capsules can be retrieved through traditional endoscopy or dissolved with medication, though surgical removal is occasionally necessary. Some physicians perform patency capsule studies before the actual procedure in high-risk patients. These dissolvable capsules test whether the actual camera capsule can pass safely.
The procedure isn’t suitable for everyone. Patients with known or suspected intestinal obstructions, severe gastroparesis (delayed stomach emptying), swallowing disorders, or certain implanted medical devices may not be candidates. Pregnancy is also a contraindication, primarily due to lack of safety data rather than known risks.
Cost and insurance coverage present challenges for some patients. While most insurance plans cover capsule endoscopy when medically indicated, prior authorization is often required. The procedure generally costs more than traditional endoscopy, and some patients face higher out-of-pocket expenses.
Interpretation requires specialized expertise. Not all gastroenterologists have extensive experience reading capsule endoscopy studies, and subtle findings can be missed or misinterpreted. This has led many centers to develop specialized reading protocols and use artificial intelligence assistance for more accurate diagnosis.
Safety Profile and Success Rates
Capsule endoscopy has an excellent safety profile with serious complications being extremely rare. The most comprehensive studies show adverse event rates below 1%, making it one of the safest diagnostic procedures in gastroenterology. Most complications are related to capsule retention in patients with underlying structural abnormalities.
Success rates for reaching the cecum (beginning of the large intestine) exceed 85% in most studies, with complete small bowel examination achieved in the vast majority of cases. Factors affecting success include gastric emptying speed, intestinal motility, and individual anatomical variations.
Diagnostic yield varies by indication but consistently outperforms other imaging methods for small bowel evaluation. For unexplained gastrointestinal bleeding, diagnostic yields range from 40-70%, significantly higher than other non-invasive tests. For Crohn’s disease evaluation, capsule endoscopy detects small bowel involvement in 70-80% of patients with negative conventional imaging.
Future Developments and Innovations
The field continues to evolve rapidly with exciting developments on the horizon. Researchers are developing capsules with enhanced imaging capabilities, including narrow-band imaging for better tissue characterization and zoom capabilities for detailed lesion examination.
Real-time viewing systems are being tested, allowing physicians to monitor the capsule’s progress and potentially control its movement or imaging parameters. Some experimental capsules include biopsy capabilities, though these remain in early development stages.
Artificial intelligence integration is advancing quickly, with machine learning algorithms showing promise for automated lesion detection and classification. These systems may eventually provide real-time alerts during procedures and improve diagnostic accuracy while reducing reading time.
Targeted drug delivery represents another frontier, with capsules designed to release medications at specific intestinal locations based on pH, time, or other triggers. This could revolutionize treatment for inflammatory bowel disease and other localized intestinal conditions.
Making the Right Decision
Capsule endoscopy represents a significant advancement in digestive health diagnostics, offering comprehensive small bowel examination without traditional procedure discomfort or downtime. For patients with unexplained bleeding, suspected inflammatory bowel disease, persistent digestive symptoms, or concerns about invasive procedures, this technology provides answers previously difficult to obtain.
The procedure’s patient-friendly approach eliminates many barriers that prevent people from seeking necessary diagnostic testing. Success stories abound of patients finally receiving diagnoses after years of uncertainty, leading to appropriate treatment and symptom resolution.
Consider discussing capsule endoscopy with your gastroenterologist if you have unexplained iron deficiency anemia, suspected small bowel Crohn’s disease, persistent abdominal pain with negative conventional testing, or if you’re anxious about traditional endoscopic procedures. Your physician can evaluate whether you’re a good candidate based on your specific symptoms, medical history, and risk factors.
This innovative technology proves that sophisticated medical diagnostics can prioritize patient comfort while maintaining diagnostic accuracy. The future of digestive health diagnostics is becoming increasingly patient-centered, with capsule endoscopy leading the way in making essential medical testing more accessible and less intimidating.
Getting crucial answers about your digestive health can be as simple as swallowing a pill and continuing your normal day – a remarkable achievement that’s helping thousands of patients find answers and peace of mind.
